Comprehensive Palliative Care
for Serious Illness
Prioritizing the Patient
PROJECT TEAM
Dean Higgins, Project Lead
Senior Director, Business Operations
Connect
Emily Roland, Project Lead
State Director, NC Implementation Team
Connect
Karen Reynolds
State Director, SC Implementation Team
Connect
Miriam Tardif-Douglin
Program Manager, Research & Policy
Madison Ward Willis
Planning Manager
Jai Kumar, Project Lead
Deputy Director
PROGRAM RESOURCES
Prioritizing the Patient: An Individualized Approach to End-of-Life Care
Comprehensive Palliative Care for Serious Illness Care Framework
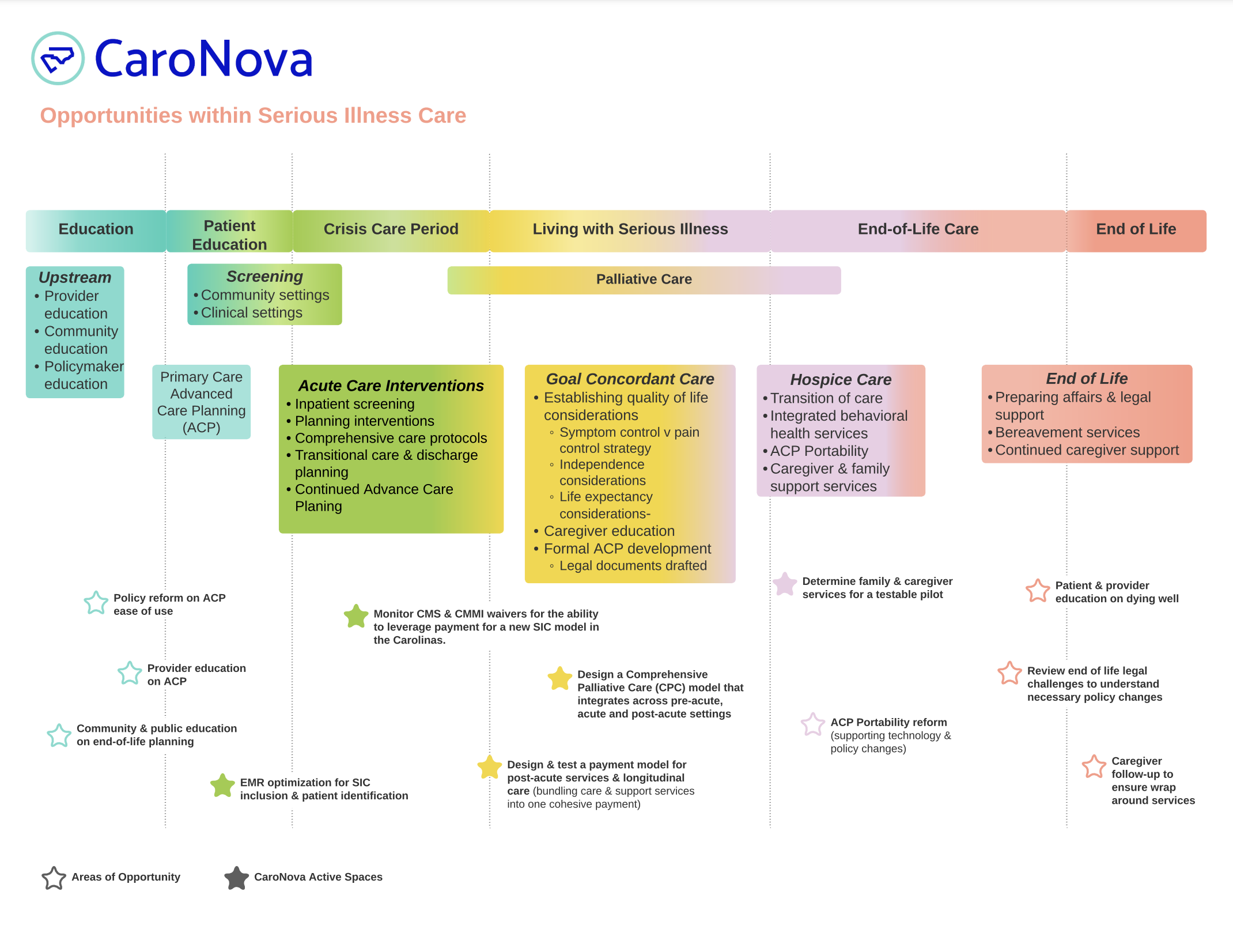
Opportunities Within Serious Illness Care
Serious Illness Care Patient Journey Map
Project Overview
Issues impacting people who are seriously ill — some of them at the end of their lives — and those who love and care for them can be emotionally, physically, and financially daunting.
At CaroNova, we are working to design a new system to provide patients and caregivers with healthcare options to help them navigate this challenging time with as much grace, dignity, and ease as possible. Working with our healthcare partners to design, test and revise a new comprehensive care model and payment infrastructure system to support and care for the seriously ill across the Carolinas, our ultimate goal is to improve their quality of life.
Launched in 2020, was an initial sustained area of focus for us. We have convened a working group that includes patient advocates, clinicians, payors, and hospital finance executives. Our workgroup members are all using their expertise to co-design these new structures as well as a robust system to pilot and test them.
Why Comprehensive Palliative Care Improvements are Needed in the Carolinas
Experts define serious illness as any health condition with a high risk of mortality that impedes a person’s daily functioning or quality of life, or “excessively strains” their caregivers. Patients with serious illnesses can be of any age.
Serious illness includes diagnoses such as kidney disease, heart disease, and dementia. In 2020, almost 14,000 people in South Carolina alone were living with end-stage kidney disease. Such conditions take a heavy toll on those living with them. That following year, more than 30,000 North Carolinians went to the emergency department for congestive heart failure and more than 18,000 for advanced dementia. People living with serious illness and their families need a special level of care.
“Palliative care is appropriate at any age and any stage in a serious illness, and it can be provided along with curative treatment.” — Center to Advance Palliative Care
Palliative care improves patient quality of life while reducing time spent in the hospital. Two defining elements of palliative care are (1) sensitive communication about disease prognosis and end-of-life care, and (2) safe symptom management (e.g., pain, nausea). Nonetheless, according to the Center to Advance Palliative Care, patients with serious illnesses report 3 major barriers:
Poor experience of care: In a 2018 national survey of more than 1,400 respondents, less than half were asked about the care they wanted if their health precipitously declined and almost a quarter (23%) got conflicting direction from their care team.
When consulted about their experience with serious illness, patients across North and South Carolina reported pausing treatment “out of frustration.”
Financial uncertainty: Despite largely being insured, more than a third (37%) of the 2018 survey respondents with serious illness reported nearly depleting their savings.
Overwhelmed caregivers: Patients consulted in the Carolinas who have serious illnesses recalled wondering, “How will this impact my family?” In addition, more than a third (36%) of those surveyed at a national level and supported by family caregivers reported they saw visible strain in their caregivers as a result.
Racial Disparities: Most Medicare patients indicate a preference not to die in the hospital or receive intensive care, yet a disproportionate share of Black patients die under these conditions.
CaraNova and the healthcare partners we work with believe that dying with dignity means treating the patient as an individual and providing the appropriate support necessary for a patient or caregiver to make decisions around their own end-of-life care. We also believe that all Carolinians deserve the right to die with dignity and that providers and payors in North and South Carolina are both interested in improving end-of-life outcomes. Healthcare professionals can coordinate appropriate resources and remove barriers limiting patients and caregivers from taking a more active role in decisions — medical or otherwise — to meet the patient’s expectations of what a “death with dignity” means for them. Payors can create a reimbursement structure that supports the appropriate utilization of services — customized to the individual — for greater patient and provider satisfaction. By bringing together key stakeholders like providers, payors, and patients to identify and enable common goals around end-of-life care for the seriously ill, we have a life-changing opportunity to reimagine a system that is inclusive, patient-centered, and delivers better outcomes for all.
CaroNova and Healthcare Partners Catalyzing Change: New Models of Care and Care Payment Will Soon Be Piloted
In late 2022, CaroNova and its partners released a recommendation report for CPC for Serious Illness detailing the elements of the care model, the requisite healthcare staffing and the principles of an alternative payment model to support it. The report served as a guide for the development of a demonstration project.
To date, we have:
-
-
Worked alongside payor and provider partners to co-design a pilot to test and validate the CPC model.
-
Laid the groundwork for an alternative payment model (APM) based on input from palliative care providers including health systems and community-based organizations across the Carolinas and discussions with payor partners. This model will be tested during the pilot.
-
Further defined and refined CPC program requirements, criteria for participation (e.g., existing palliative care infrastructure), expectations for collaboration, technical assistance elements and data collection and reporting requirements for the pilot.
-
Learned from the provider partners the equally critical importance of establishing cross-continuum partnerships and alignment as a criteria for readiness.
-
Been advised by provider partners on the types and levels of implementation support sites may receive through our state technical assistance teams, including significant onboarding support and peer-to-peer learning opportunities within the pilot.
-
Engaged a private payor to serve as a thought partner on the APM design in conjunction with other payor groups in North and South Carolina. These discussions have centered around establishing the business case for the CPC model, presenting case studies on relevant APM models and projects, and receiving feedback on the proposed metrics and evaluation plan. Based on payor and provider feedback to date, the APM will be developed in a phased approach throughout the pilot. The first phase will focus on confirming the case rate with grant support; subsequent phases will evaluate the addition of quality incentives and risk sharing under value-based contracts.
-
We are continuing to engage pilot design partners and will collate findings and recommendations from these groups to finalize the overall pilot framework. We will soon release the targeted request for proposal and identify and onboard pilot sites.
We will confirm the feasibility of implementing and scaling the CPC model for payors and providers, thereby informing the next phase of the demonstration. As a result of these efforts, we ultimately aim to establish a sustained payment mechanism for CPC for Serious Illness in the Carolinas.
Sources
- North Carolina Patient Data System
- 2019 Center to Advance Palliative Care “America’s Care of Serious Illness” https://reportcard.capc.org/wp-content/uploads/2019/09/CAPC_ReportCard19-Digital_9_19.pdf
2019 Kelley, AS, “Identifying the Population with Serious Illness: The “Denominator” Challenge” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5756466/#:~:text=Conceptual%20Definition-,%E2%80%9CSerious%20illness%E2%80%9D%20is%20a%20health%20condition%20that%20carries%20a%20high,OR%20excessively%20strains%20their%20caregivers. - 2018 The Commonwealth Fund, “Being Seriously Ill in America Today” https://cdn1.sph.harvard.edu/wp-content/uploads/sites/94/2018/10/CMWF-NYT-HSPH-Seriously-Ill-Poll-Report.pdf
- 2021 US Census Bureau “American Community Survey” https://data.census.gov/table?t=Disability&g=040XX00US37,45&tid=ACSST1Y2021.S1810
- US Census Bureau, “Guidance for Disability Data Users” https://www.census.gov/topics/health/disability/guidance/data-collection-acs.html#:~:text=Self%2Dcare%20Disability%20Because%20of,getting%20around%20inside%20the%20home.
- 2021 American Kidney Fund, “Kidney Failure (ESRD) in South Carolina” https://www.kidneyfund.org/sites/default/files/media/documents/South-Carolina-April-2021.pdf